Are you using a diabetes device that has a calculator to work out your insulin doses?
- APP’s: MySugar, Diabetes:M, Dario etc.
- Glucose meters: Insulinx, Freestyle Libre etc.
- Pumps: Omnipod, Medtronic, Animas, all others except ROCHE pumps.
If so you need to know about Active Insulin, or as it’s commonly known, Insulin on Board (IOB).
To get specific, you need to know:
- How many hours IOB should be set at, so your calculator gives the right correction doses.
- How you can use IOB to improve blood glucose control around exercise.
- How different devices calculate IOB differently and how this can impact your glucose control.
These are all things I wanted to know when I was choosing an insulin pump six years ago. But no one knew the answer, well not a satisfactory one anyway. So I undertook a journey of delving through John Walsh’s “Pumping Insulin”, Gary Scheiner’s “Think like a pancreas” and read all the manufacturers’ operation manuals to find out.
At its most basic level, IOB refers to how much insulin from the bolus you have recently delivered is still working in the body. Most devices use a linear model to determine how the IOB degrades in your body over time.

Simply if IOB is set at 4 hours and 4 units are administered the device will think:
- Just after bolus there are 4 units left
- After 1 hour 3 units left
- After 2 hours 2units left
- After 3 hours 1 unit left
- After 4 hours 0 units left.
Some devices such as Medtronic use a curvilinear approach BUT this is very similar to the linear model. Most manufacturers set IOB at 4 hours (range 2-8 hours) as default, and most diabetes services suggest starting at 4 hours.
But is this the best setting for you?
The IOB information can be used in two main ways:
- For blood glucose meters, APPS, and pumps to prevent the user from delivering too much correction insulin for a high glucose level in the 1-4 hours after eating.
I shall show you the maths in a minute.
- For the user to see how much insulin is still working from the previous bolus when the user is about to undertake an activity.
This helps determine if they need to do a bolus or not for intense (anaerobic) activity, or if they need more carbohydrate than usual for endurance (aerobic) or even intermittent (team sports) activity.
It is very useful here to stop and think about the main reason you want to use IOB.
- To help workout correction doses between meals using the calculator in your APP/device?
Or,
- To use to help guide exercise decisions by knowing how much IOB you have, and therefore your hypo risk?
You may be wondering why you need to choose. It will become clear as you read on.
Before we go any further I want to clarify I am talking about the quick acting insulin’s: NovoRapid, Humalog, Apidra, Fiasp.
If you look at their profile:
- Peak action is about one hour
- The total duration of action is 4-6 hours depending on the volume of the dose.
o A high dose: 0.25u/kg – for me weighing 100kg would be 25 units and would last 6 hrs.
o A smaller dose of 0.1u/kg – for weighing 100kg would be 10 units and would last 4 hrs.
Make a special note that the above is from published studies on insulin action and it’s very consistent for people with type 1 diabetes. However, that does not mean you should set IOB in your device at 4-6 hours.
Remember, fast acting insulin does actually last 4-6 hours in the body.

How does IOB prevent over corrections between meals?
Have you ever gone to correct a high glucose one, two or three hours after eating, and your device says no correction, even though you know you need one?
Sound familiar?
This sections will explain why, and offer some solutions.
Most diabetes technology (Except ROCHE devices: ROCHE pumps and Expert meter – which I will address in a future post) use IOB to prevent over correcting in-between meals. They do this by registering how much insulin was given for the carbs and correction at the last meal and then using an algorithm for IOB to predict how much is still working in the body. This amount left as IOB is then deducted from the potential correction required. Remember these algorithms are linear in nature as described above, and most IOB is set at 4hrs.
Examples for mmol/l and mg/dl below:
Mmol/l – A bolus of 10 units was given 2 hours ago for 100g carbs at 1u:10g, so via the algorithm the device thinks there is still 5 units IOB after two hours (set at 4 hours). The person’s Sensitivity factor is 1u reduced BG by 2mmol/l – therefore the device thinks that potentially the glucose could drop by 10mmol/l.
Current BG 15.0mmol/l – target is 5.0mmol/l = it needs to drop by 10.0mmol/l and sensitivity factor is 1u:2mmol/l – therefore 5units correction needed. But, there is 5 units IOB so no correction is offered.
Can this be right, no correction for a BG of 15mmol/l at 2 hours!
Mg/dl – A bolus of 10units was given 2 hours ago for 100g carbs at 1u:10g, so via the algorithm the device thinks there is still 5 units IOB (set at 4 hours). The person’s Sensitivity factor is 1u:36mg/dl – therefore the device thinks that potentially the glucose could drop by 180mg/l.
Current BG 270mgl/dl – target is 90mg/dl = it needs to drop by 180mg/dl and sensitivity factor is 1u:36mg/dl – therefore 5units correction needed. But, there is 5 units IOB so no correction is offered.
Can this be right, no correction for a BG of 270mg/dl at 2 hours!

Here’s the reason why THIS IS A MASSIVE PROBLEM:
The devices do not understand the 5 units IOB are actually accounted for by the 50g of carbs still sat in the stomach, waiting to be digested. Therefore, no correction is given and the glucose is still high in another two hours’ time.
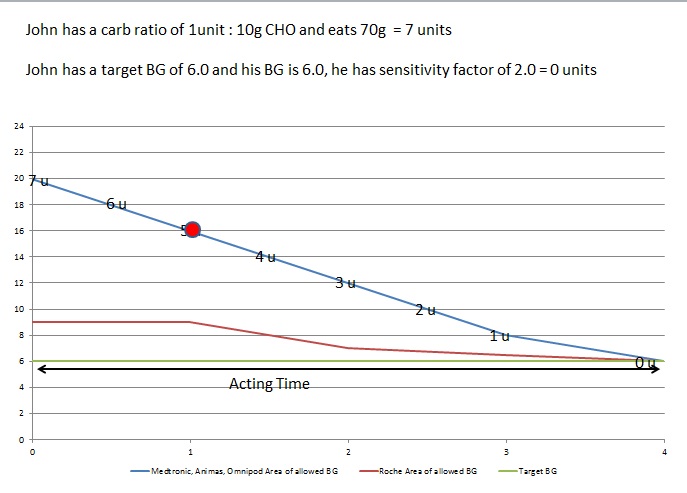
The picture below shows that no correction would be offered for BG of 22.00mmol/l (396mg/dl) one hour after eating because IOB is set at 4 hours, and the device still thinks that the 5 units IOB could bring the glucose down by 10mmol/l (180mg/dl), because the Sensitivity factor is 2.0mmol/l (36mg/dl).
What it should be thinking is the 5 units is accounted for by the 50g of carbohydrate still waiting to be digested in John’s stomach.
Pic 1:
The next shows that only 4.5 units correction would be offered for BG of 22.0mmol/l ( (288mg/dl) two hours after eating because IOB is set at 4 hours, and the device still thinks that the 3.5 units IOB could bring the glucose down by 7mmol/l (126mg/dl), because the Sensitivity factor is 2.0mmol/l (36mg/dl).
What it should be thinking is the 3.5 units is accounted for by the 35g of carbohydrate still waiting to be digested in John’s stomach.
Pic 2:
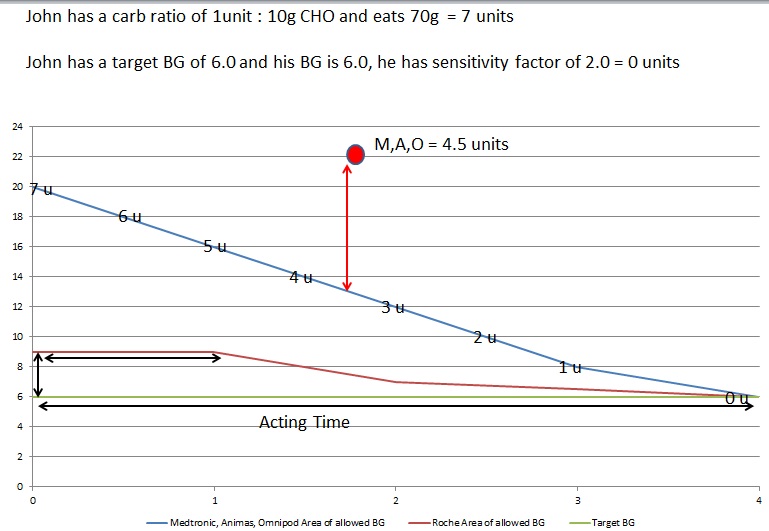
Pictures 1 and 2 show how a correction will only be offered to correct to the outer edge of the triangle, where the IOB degrades in a linear fashion, where the outer edge of IOB is determined by the hours the IOB is set at.
See picture 3 below, where it shows the outer edge where IOB is set at 2-5 hours. This graph also gives a good hint as to why the ROHCE devices have a much better algorithm when it comes to correcting high glucose levels.
Pic 3
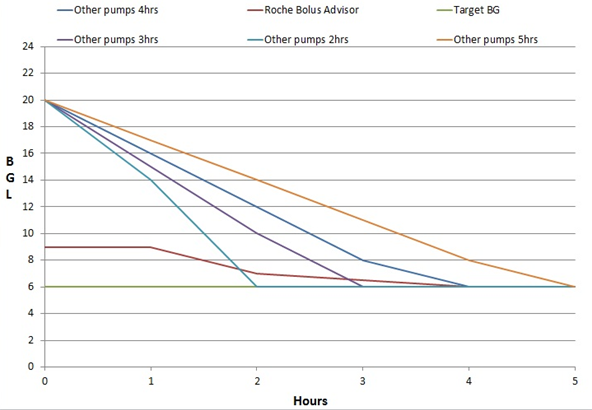
The simple take-home for this graph is:
- The shorter the IOB, the more aggressive the corrections.
- The longer the IOB the less aggressive the corrections.
Where should it be set?
- 4 hours for most people is too long and means they do not get the necessary corrections in-between meals. However, if you are a hypo risk person maybe this would be safe for you, but it would lead to higher hba1c.
- 2 hours is probably too short as, if a correction is done at 2 hours the pump will think no IOB and give the full dose to bring to target. You may miss out on a bit of protection.
- The sweet spot is 2.5 to 3 hours, 2.5 is more aggressive, 3 hours more conservative. Some devices only do hourly options.
A few important points are the type of behaviours that do better with shorter IOB times and those for longer IOB times:
Shorter IOB times 2-3 hours:
- Low carb diets
- Bolus 15 mins before meals
- Choose Low Glycaemic index carbs
- Have good hypo awareness
Longer IOB times 3-4 hours:
- Bolus after meals
- Choose High Glycaemic index carbs
- Hypo unaware
ALWAYS CHECK WITH YOUR MEDICAL TEAM BEFORE CHANGING ANYTHING.
Using IOB for exercise management.
Here lies the conundrum. We know the actual duration of insulin is 4-6 hours but we have to set IOB to 2.5 – 3hrs so it allows effective corrections. This means if set at 2.5 hours and you exercise at 3 hours after eating, you look at IOB and it says 0units – you think great no bolus insulin to consider, crack on…
This often leads to a hypo if doing aerobic activity, because there is some insulin still working for the previous bolus. If you knew there was still 1.5 units in the body, you would have had more carbs.
This often leads to hypo if doing aerobic activity, because there is some insulin still working for the previous bolus. If you knew there was still 1.5 units in the body, you would not have given the extra 1 unit you thought you needed to prevent a BG spike.
If IOB was set at 4-6 hours it would let you know how much is really still working, which is great for exercise, BUT you would never be able to correct between meals.
So the real question to ask is what you want to primarily use IOB for, correcting, or for exercise?
If for correcting primarily:
- Set IOB at 2.5-3 hours to allow effective corrections.
- Be aware when exercising 2.5-4 hours after a bolus there will be IOB but the device will read 0units. But there will be insulin still working that needs considering in your exercise plans.
If for exercise primarily:
- Set IOB at 4-5 hours and this will be a good estimate of how much is still working in the body.
- Override the correction suggestions by the device to give more correction, or calculate your doses manually using your sensitivity factor.
If for both:
- Set at 3 hours and you get a half-way house for both corrections and exercise. This could be the most sensible option, but could also get the worst of both worlds.
The way the ROCHE meters and pumps calculate IOB is much better and allows very sensible and effective correction doses, BUT is useless for exercise, as you cannot see the IOB effectively. Another article, for another time.
Hope this has helped.
ALWAYS CHECK WITH YOUR MEDICAL TEAM BEFORE CHANGING ANYTHING.
If you liked this article and want to learn more about insulin dosing strategies for better diabetes, then check out the Diabetic Muscle and Fitness Training Lab.
It contains a vault of in-depth knowledge and resources you can’t find anywhere else on the internet.
Join 1000s of other diabetics just like you. Ask questions, learn and start building the body you have always dreamed of.
Written by Head Coach at Diabetic Muscle and Fitness, John Pemberton – Diabetes Specialist Dietitian/Educator.


